“Understanding and Managing GERD: A Casual Guide”
GERD, also known as gastroesophageal reflux disease, is that annoying thing when stomach acid decides to make a U-turn back into your esophagus. Thanks to this rebellious stomach acid, many people experience heartburn, a fiery sensation that starts in the chest and can travel up to the throat and neck. It’s like your body’s own version of a volcano, and it can cause quite a stir if not managed properly.
So, what exactly is GERD? Think of it this way: there’s a valve called the lower esophageal sphincter (LES) that acts as the gatekeeper between your esophagus and stomach. When this gatekeeper gets lazy or decides to take a break at the wrong time, stomach acid can sneak back into the esophagus, causing irritation and inflammation. It’s not meant to be there and can be pretty corrosive, leading to that uncomfortable burning sensation.
Heartburn is the standout symptom of GERD, but it’s not the only guest at this party. Along with the burning chest pain, other symptoms might crash the event: there’s the sour or bitter taste in your mouth, issues swallowing, pesky nausea, bad breath, and sometimes even a feeling like you’ve got a lump in your throat. Left unmanaged, GERD might even affect other parts beyond your esophagus, leading to a cough, wheezing, hoarseness, or chest congestion, and could aggravate conditions like bronchitis or asthma.
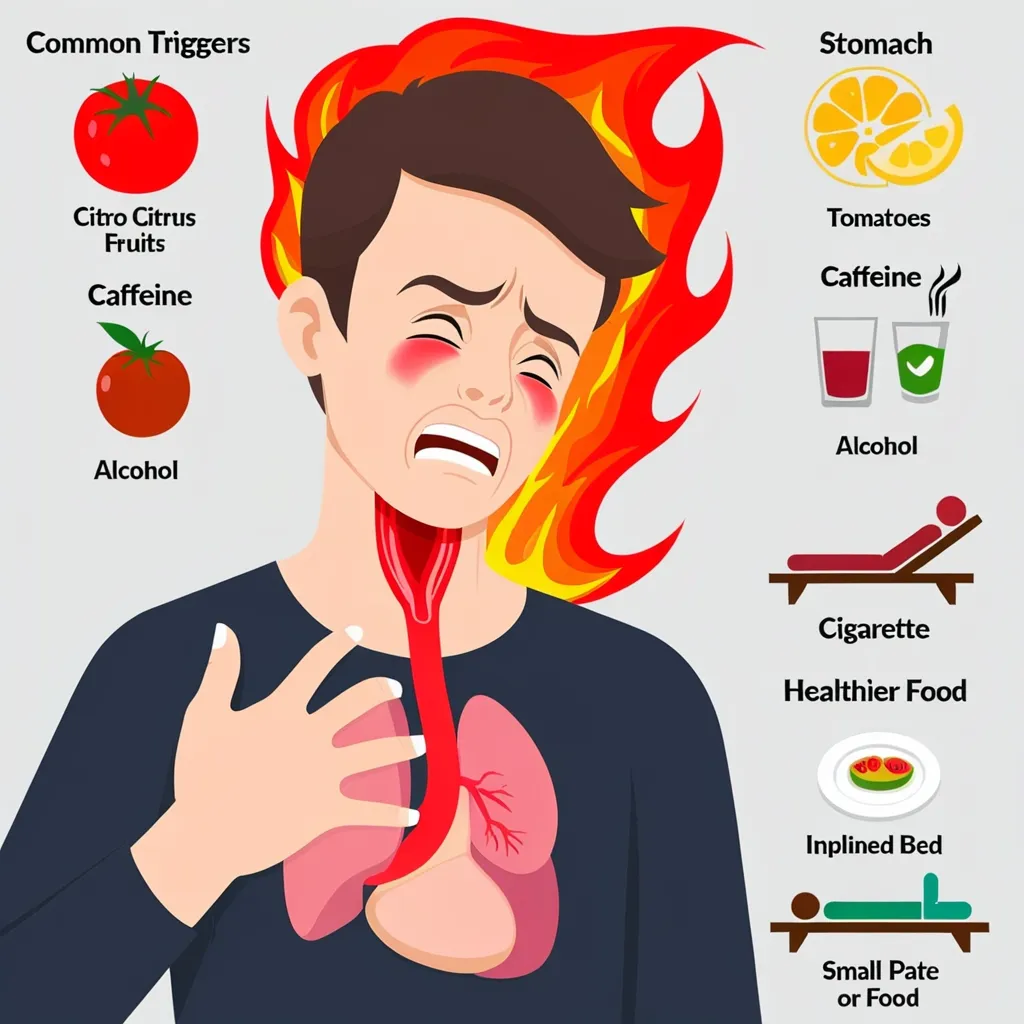
Adjusting your lifestyle can be a game-changer if you’re living with GERD. One of the key things is to shed those extra pounds if you’re carrying a few extras. Excess weight can press down on your stomach, encouraging the LES to slack off even more. Changing what goes on your plate is crucial too. Steering clear of foods that ramp up acid production, such as caffeinated drinks, citrus fruits, and tomatoes, can be a lifesaver. And those fatty foods, alcohol, and peppermint? They make the LES as lazy as a snoozing cat, so it’s best to avoid them. Smaller, frequent meals can also help keep the acid in check.
Other tips to keep GERD at bay include kicking the smoking habit, waiting a bit before lying down after a meal, and propping up the head of your bed by about 6 to 8 inches. These tweaks can reduce the chances of acid making a comeback into your esophagus.
When lifestyle changes aren’t cutting it, medication is usually the next stop. Starting with antacids, you can find relief by neutralizing stomach acid. They’re great for those occasional flare-ups but be cautious with their frequent use due to possible side effects like diarrhea. Histamine 2 blockers are another option and work by reducing acid production. They can be grabbed over-the-counter or through a prescription.
Proton pump inhibitors (PPIs), on the other hand, are the heavyweights in acid suppression. They’re top of the class in reducing acid and healing the esophagus from erosive damage. Over-the-counter or prescription, medicines like omeprazole (Prilosec), esomeprazole (Nexium), and lansoprazole (Prevacid) are some common examples.
Then there are prokinetic agents, which help your digestive system move along more swiftly, quite literally fast-tracking food through your system, often used alongside other acid-suppressing meds.
If lifestyle changes and medication still aren’t cutting it, endoscopic therapy can be an option. Techniques like transoral incisionless fundoplication (TIF) use an endoscope to reconstruct a better barrier to keep stomach acid out. This less invasive procedure offers quicker recovery and less pain compared to traditional surgeries.
Sometimes, though, surgery is the way to go. The go-to surgical option is the Nissen fundoplication, where the upper part of the stomach is wrapped around the lower esophagus to bolster the anti-reflux barrier. It’s often done laparoscopically, meaning less invasive procedures with quicker recovery times.
Ignoring GERD isn’t a great idea because it can lead to some gnarly complications. Chronic acid reflux can irritate the esophagus, leading to esophagitis or Barrett’s esophagus. Severe untreated cases might even end up with painful ulcers. Long-term management often requires a combo of lifestyle tweaks and medication. For some, surgery is the ultimate answer to bid farewell to symptoms.
Wrapping it all up, GERD is one of those conditions that you can manage pretty well with some proactive steps. From changing what you eat to perhaps popping a pill, or sometimes even opting for surgery—there’s a range of strategies to keep that stubborn stomach acid in check. By understanding what triggers it and learning about the variety of solutions, individuals can take control and wave goodbye to that irritating discomfort for good.