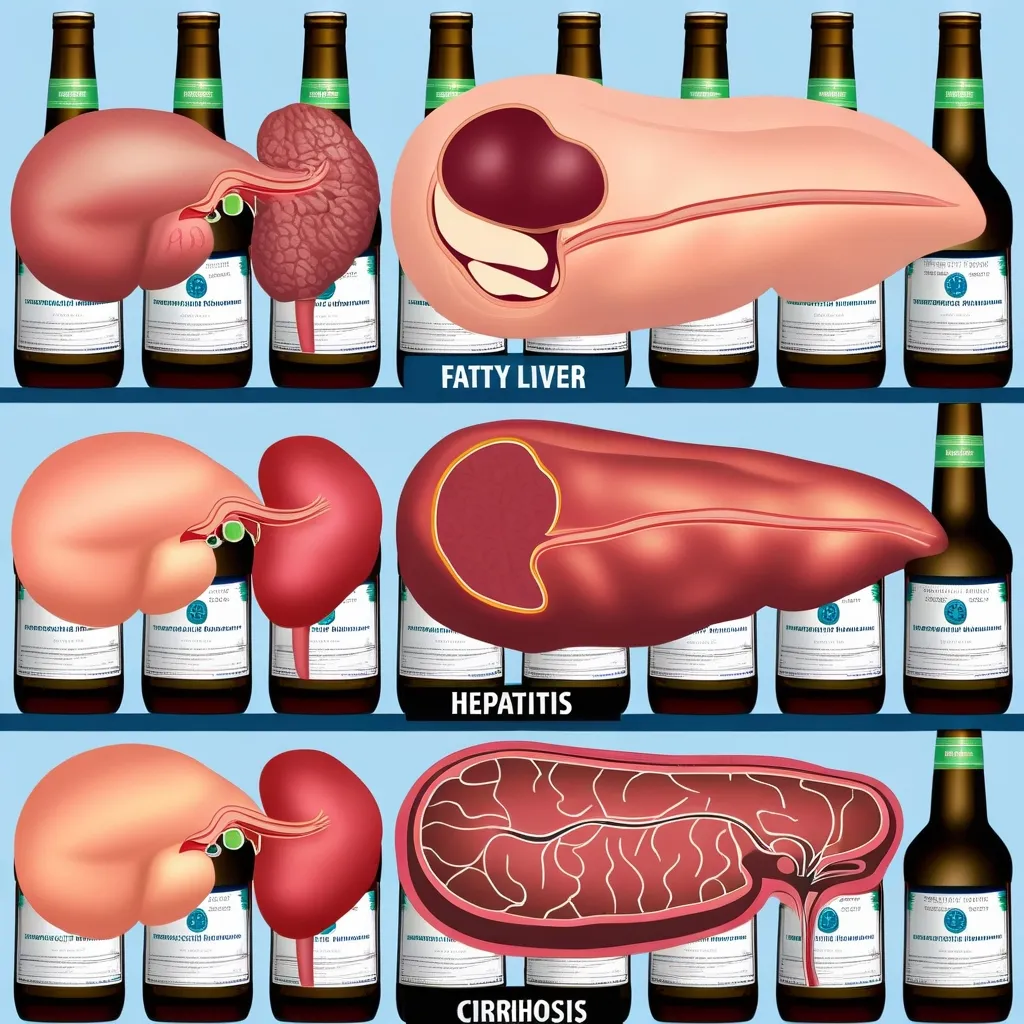
Alcohol-induced liver disease (AILD) is no joke. It’s a serious condition that pops up when you’ve been knocking back too many drinks for too long. The liver, your body’s detox powerhouse, gets overwhelmed and starts to rebel. This rebellion shows up in different forms like fatty liver, alcoholic hepatitis, and cirrhosis, each with its own set of symptoms and ways to tackle it.
First off, let’s talk about how AILD progresses. When you drink alcohol, your liver gets to work processing it. But when you drink too much, too often, your liver can’t keep up. The first sign is usually a fatty liver, where fat builds up in the liver cells. Most people don’t even realize this is happening because it doesn’t really show any symptoms. Sometimes, you might feel a bit of discomfort in the upper belly or just generally tired. But if you keep drinking, things can get worse and lead to alcoholic hepatitis, which means your liver is inflamed and damaged.
Now, how can you tell if it’s alcoholic hepatitis? This one ramps up pretty quickly. You might notice jaundice, which is just a fancy word for yellowing of the skin and eyes. You’ll probably feel pretty crummy, with symptoms like weakness, stomach pain, nausea, and loss of appetite. If it gets really bad, you could end up with complications like bleeding in your gut, fluid building up in your belly (called ascites), or even confusion due to something called hepatic encephalopathy.
To figure out if someone has alcoholic hepatitis, doctors usually rely on a mix of your health history, a physical check-up, and a bunch of tests. Blood tests are big here because they can show how much liver damage there is. They might also use imaging tests like ultrasounds, CT scans, or MRIs to get a good look at your liver. Sometimes, they need to do a liver biopsy to be sure.
The main treatment for alcoholic hepatitis is to completely stop drinking alcohol. This is the only way to stop the disease from getting worse and give your liver a chance to heal. If it’s a mild case, you might not need to go to the hospital, but you will need to be watched closely. Good nutrition is crucial, so things like vitamins and minerals, especially folate and thiamine, are important. For those with bleeding issues, Vitamin K can help.
In more severe cases, you might need to be hospitalized and possibly even require intensive care. Doctors sometimes use medications like glucocorticosteroids to try to reduce liver damage and inflammation, but there’s some debate on how effective these drugs are. Other treatments, such as pentoxifylline, are also being looked at.
Making some lifestyle changes is key to recovering from alcoholic hepatitis. You should steer clear of fatty foods since they can make things worse for your liver. It’s essential to stick to a balanced diet and keep up with regular check-ups with your healthcare provider. Joining treatment programs for alcohol use disorder, like Alcoholics Anonymous, can really help with staying sober.
If you don’t stop drinking, alcoholic hepatitis can spiral into cirrhosis, where the liver gets badly scarred. Cirrhosis can lead to liver failure, and at that point, you might need a liver transplant. But getting a transplant usually means proving that you’ve stayed away from alcohol for a while, often about six months.
People with alcoholic hepatitis also have to be on the lookout for other problems like infections, kidney failure, and liver cancer. Keeping an eye on things with regular check-ups is crucial. Vaccinations against things like hepatitis A and B, the flu, and pneumococcus are recommended to prevent infections.
Looking ahead, there’s a lot of research going on to better understand alcoholic hepatitis and develop more effective treatments. Some of the exciting new directions include gene therapy, targeting the genes that play a role in liver fibrosis and inflammation.
The takeaway here? Early recognition of alcoholic hepatitis is super important for better outcomes. Many heavy drinkers don’t realize they’re damaging their livers until it’s pretty far gone. Regular health check-ups and being open with doctors about alcohol use can help catch things early and make a big difference.
In summary, alcohol-induced liver disease is something you can prevent. It needs immediate attention and a serious commitment to changing your lifestyle. Quitting alcohol completely, together with good nutrition and proper medical care, is the way to go. Spotting the disease early and acting fast can make a huge difference in the long run.