Strokes are a serious business. When blood stops flowing to the brain, it can cause major problems, including brain damage and even life-threatening situations. There are two main types of strokes: ischemic and hemorrhagic. They’re both nasty, but they mess you up in different ways.
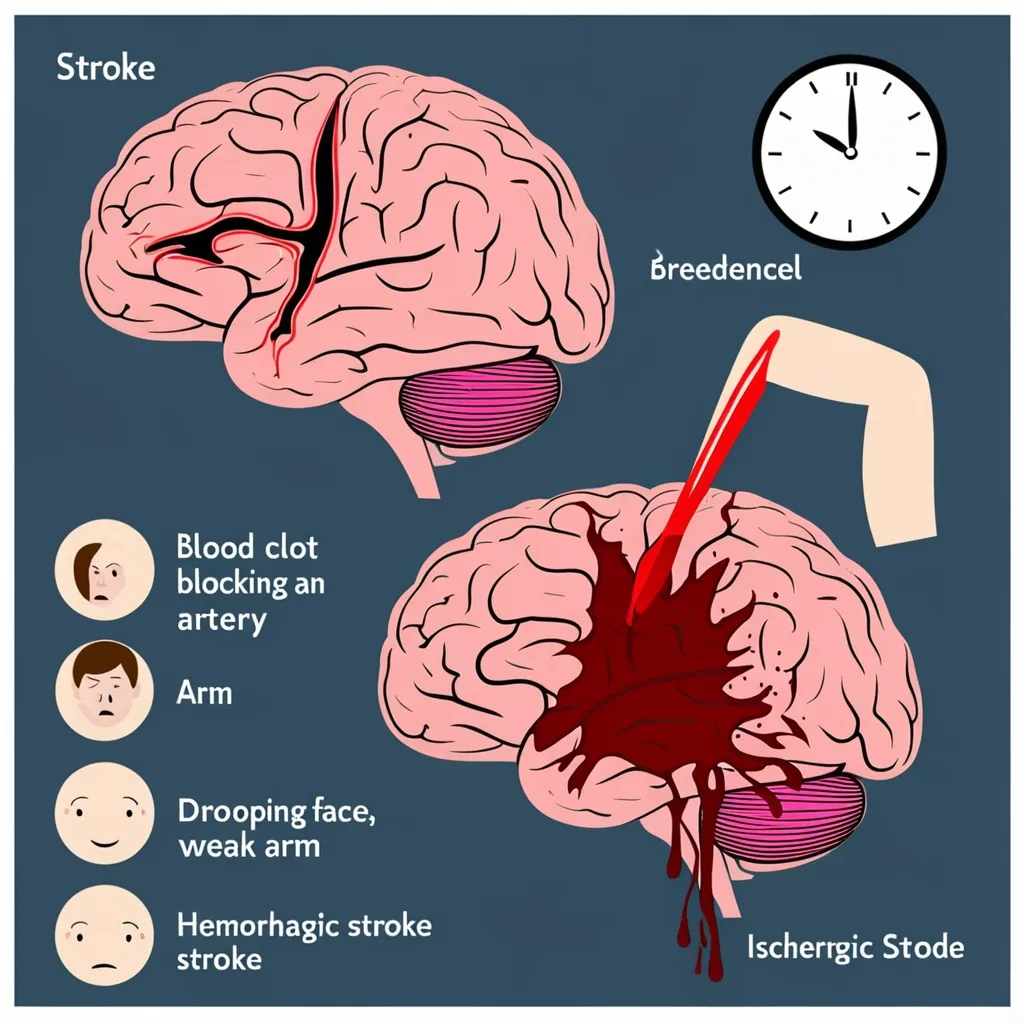
Ischemic strokes are the more common of the two, making up about 85% of all stroke cases. These happen when a blood clot clogs up an artery in the brain, cutting off the blood supply and oxygen. Hemorrhagic strokes are less common but often more severe. These occur when a blood vessel bursts in the brain, leading to bleeding in the surrounding tissues. Either can be devastating, but hemorrhagic strokes tend to pack an even bigger punch.
The symptoms of a stroke can hit like a ton of bricks and can vary depending on which part of the brain is getting shortchanged on blood. Look out for sudden signs like weakness or numbness on one side of the body—whether it’s in the face, arm, or leg—along with slurred speech, confusion, dizziness, loss of balance, sudden severe headaches, nausea, vomiting, and even seizures. It’s not one-size-fits-all, but these are pretty common red flags.
When it comes to a stroke, time is of the essence. Acting quickly can be the difference between recovery and serious permanent damage. Remember the acronym FAST to check for key symptoms:
- Face: Ask the person to smile. See if one side of the face droops.
- Arm: Ask them to raise both arms. Watch for one arm drifting downward.
- Speech: Ask them to repeat a simple sentence. Notice if their speech is slurred or hard to understand.
- Time: If you spot any of these signs, don’t wait. Call emergency services right away.
Ischemic strokes need quick action to get that blood flowing again. One way is through thrombolysis, which involves giving medications like alteplase to dissolve the blockage. But the clock is ticking—this treatment works best within about 4.5 hours after symptoms kick in. Another method is thrombectomy, a procedure where doctors use a catheter to yank the clot out of the brain. This must also happen fast, generally within the first 24 hours.
Hemorrhagic strokes are more complicated to tackle. The priority here is to stop the bleeding and reduce the pressure inside the skull. Meds might be used to lower blood pressure and help with clotting, but surgery is often necessary. This could mean clipping the burst vessel, draining fluid from the skull to ease pressure, or even using a minimally invasive “burr hole” procedure.
So, what puts you at risk of having a stroke in the first place? High blood pressure is a biggie, but it’s not the only one. High cholesterol, diabetes, smoking, obesity, and a poor diet all play their parts. Living healthily can cut down the risk significantly. Staying active, eating well, and managing any chronic conditions like hypertension and diabetes are all steps in the right direction.
Recovering from a stroke can be a tough journey. The road to recovery varies from person to person and depends on how severe the stroke was and how much brain tissue was affected. Rehabilitation might involve physical, occupational, and speech therapies to help regain as much function as possible. Additional supportive care, like IV fluids, bed rest, and managing other health problems, may also be needed along the way.
Preventing future strokes is all about addressing the root causes. Sticking to a healthy diet, getting regular exercise, quitting smoking, and taking control of chronic issues like high blood pressure and diabetes are all key. Regular check-ups with your doctor can help catch any risky changes before they become major problems.
Making life adjustments can drastically lower the risk of having a stroke. Think about loading up your diet with fruits, veggies, whole grains, and lean proteins while keeping an eye on saturated fats and sugars. Staying active with regular exercise, whether it’s walking or something else you enjoy, is crucial. Kicking the smoking habit and keeping alcohol in check are also very important.
After a stroke, follow-up care is indispensable. Healthcare providers will schedule regular visits to track recovery progress and sort out any new problems. It’s also vital to inform doctors about any changes affecting daily life, even if they don’t seem directly connected to the stroke.
Stroke survivors often face complications. For instance, cerebrospinal fluid might build up in the brain, a condition called hydrocephalus, which can cause headaches and vomiting. Surgery may be needed to place a shunt to drain the fluid. Other supportive measures, like feeding tubes, nutritional supplements, and oxygen therapy, may be necessary for short-term issues.
Life after a stroke varies widely. Recovery depends on how severe the stroke was, how quickly treatment was received, and factors like age and underlying health. While some miraculously bounce back completely, others deal with long-term disabilities. Rehabilitation and supportive care are crucial in helping survivors regain independence and improve their quality of life.
To sum things up, knowing what causes strokes, recognizing the symptoms, and understanding the treatments can make all the difference in handling this medical emergency. Keeping a healthy lifestyle, managing chronic conditions, and acting fast when symptoms show up can significantly cut down the risk and impact of a stroke.