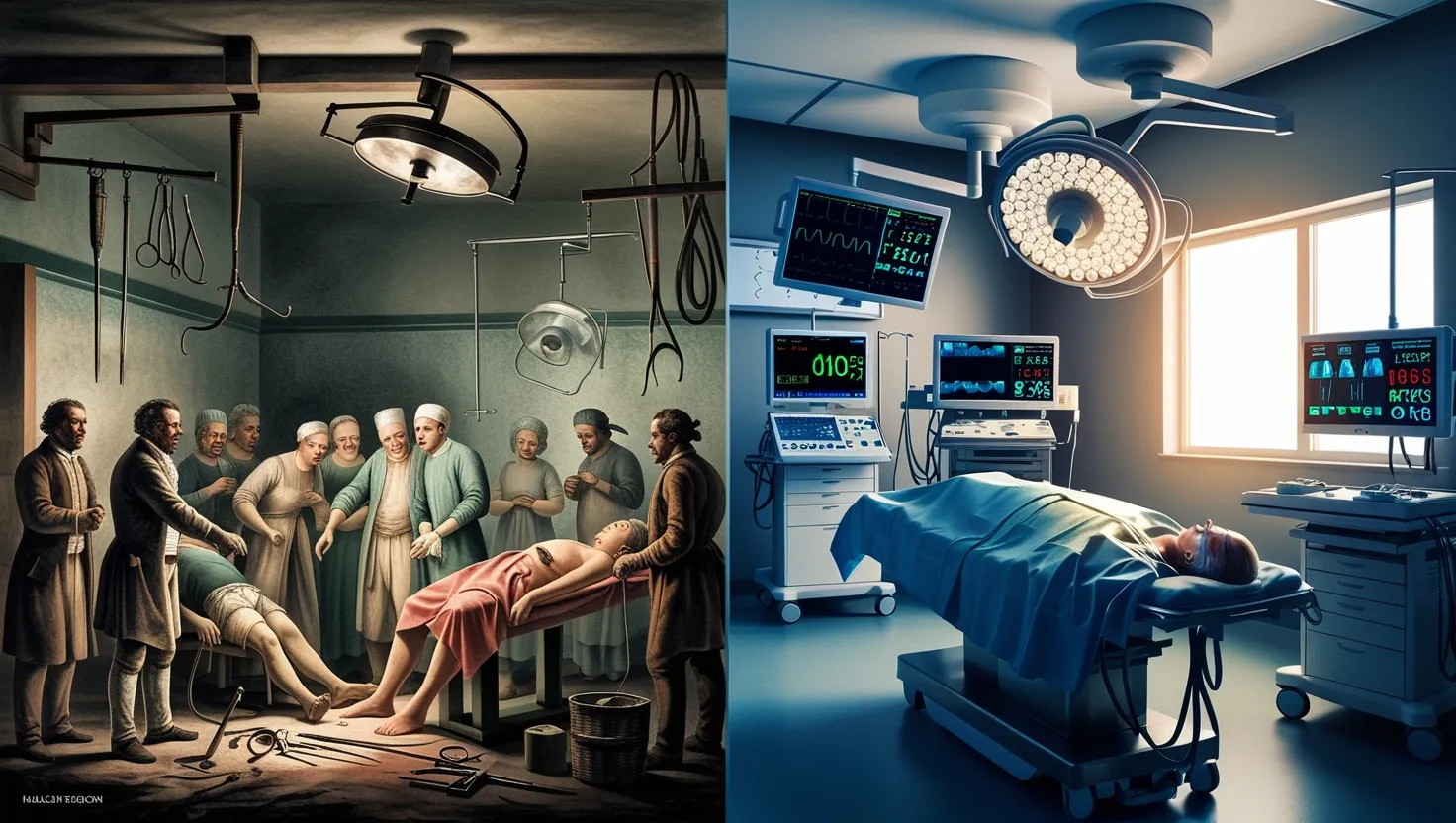
Imagine a world where surgery meant biting down on leather, feeling every slice, every tug, as doctors raced to finish before shock or infection set in. This was the reality before anesthesia transformed the operating room. Today, I want to guide you through five key anesthetic breakthroughs that changed not only surgery but the whole experience of medical healing.
Before anesthesia, pain was inevitable. Surgeons worked not just against disease, but against screams, thrashing limbs, and the certainty that their patients would remember every second. Recovery meant more than physical healing — it meant moving past the trauma of conscious surgery. How did we get from that brutal chapter in medicine to the point where surgery is painless and routine?
The first major leap took place in 1846 in the now-famous Ether Dome at Massachusetts General Hospital. When William Morton persuaded surgeons to try ether on a tumor patient, the results were so astonishing that the head surgeon declared, “Gentlemen, this is no humbug.” For the first time, the world saw major surgery conducted without agony. Ether didn’t simply dull pain: it allowed for deliberate, measured operations instead of frantic sprints. Think how that must have felt — relief not just for patients, but for surgeons long haunted by horror and helplessness. Ether quickly spread, with public demonstrations drawing crowds in America and Europe. Yet early ether users had no precise method for controlling dosage, so complications were common. Still, a new standard had been set: Pain could be managed, and surgery could be refined.
“What cannot be cured must be endured.” Before anesthesia, this adage defined medicine. But anesthesia challenged it: Could relief really be within reach?
Nitrous oxide, known widely as laughing gas, has its own quirky story. Discovered by Humphry Davy in 1799, its capacity to cause euphoria and painlessness first made it a party trick. People would inhale it for fun at social gatherings. Its transformation into a medical tool came when dentist Horace Wells saw how it dulled pain after a volunteer injured himself at a show. When Wells tried to demonstrate its surgical use, the effect was underwhelming — the patient moved, and the crowd jeered. But the seed was planted. In the decades that followed, nitrous oxide reemerged, especially in dental offices where quick pain relief and conscious patients could coexist. Its importance grew as doctors realized that shorter procedures required lighter anesthesia, making laughing gas indispensable. It’s remarkable how the very gas once dismissed on stage is now considered one of the safest forms of anesthesia, especially for dental work and childbirth.
“Science means constantly walking a tightrope between blind faith and curiosity; between expertise and creativity; between bias and openness.” The story of nitrous oxide is a testament to how curiosity, even when dismissed, can someday upend entire fields.
Chloroform entered the scene just a year after ether. James Young Simpson, a Scottish obstetrician, was on a mission to find something less irritating and more rapid than ether. With chloroform, he found a smoother ride. It caught the world’s attention when Queen Victoria famously chose chloroform for childbirth, declaring it “soothing, quieting, delightful beyond measure.” Can you imagine the change in public opinion, witnessing the Queen herself endorsing painless labor? Chloroform’s quick action and lack of harsh odor made it popular in Europe, especially for childbirth. Its story, though, wasn’t without caution. It soon became clear that chloroform could unexpectedly cause fatal heart irregularities, and for a while, the world debated: Should the possibility of relief outweigh the risk? Still, Queen Victoria’s use shifted cultural norms. Doctors and patients alike began to believe that pain in labor, once seen as essential or even virtuous, could and should be treated.
“Of all the forms of inequality, injustice in health is the most shocking and inhuman.” Although Martin Luther King Jr. spoke these words a century after chloroform’s rise, his insight matches medicine’s evolving ethos: pain is no longer a necessary experience.
Next, let’s consider a change in how anesthesia is given. Instead of putting the entire body to sleep, local anesthesia works by blocking pain in specific parts. The pivotal moment came with the isolation of cocaine in the 19th century. Carl Koller, a young ophthalmologist, needed a safe alternative for delicate eye surgery. After observing cocaine’s numbing effects, he realized it could allow operations on conscious, cooperating patients. Imagine being able to perform minute surgery — or even simple extractions — without affecting the brain or vital organs. Epidural anesthesia for childbirth and dental freezing would have been impossible without these first experiments. Eventually, much safer compounds like procaine and lidocaine expanded the reach of local anesthesia. This breakthrough quietly revolutionized outpatient medicine. No longer confined to the hospital, minor surgeries shifted to clinics and, eventually, to the patient’s bedside.
How would surgery look today without the comfort of numbing a tiny patch of skin? Would you book your next dental appointment so easily?
We’ve now arrived at the modern approach: balanced anesthesia. Early pioneers, from Morton to Simpson, worked without precise measurements. Today’s anesthesiologists combine inhaled gases, intravenous drugs, and local nerve blocks. Their aim? To induce unconsciousness, block pain, relax muscles, and control vital signs with exacting precision. Marathon operations, complex heart repairs, organ transplants, even brain surgery — all have become feasible and safe thanks to these advances. The anesthetic plan is custom built for each patient, adjusted in real time by specialists trained not just in chemistry and biology but also in the art of rapid decision-making. The anesthesiology team stands watch at the patient’s head, tracking data on screens, always ready to intervene.
“Medicine is a science of uncertainty and an art of probability.” Those words, from Sir William Osler, couldn’t be more true in anesthesia. Every advancement builds on tiny increments of progress, risks weighed against benefits, always striving toward less suffering.
Let me share with you perspectives that don’t always enter textbooks. Surgical anesthesia didn’t just reduce pain — it created a new kind of patient. No longer immobilized by agony, patients could recover without the psychological scar of torture. Surgeons, too, found new freedom to learn, improve, and tackle more complicated diseases. Yet, with each advance, new challenges emerged. The first patients sometimes developed pneumonia from ether’s toxicity, and chloroform, while gentle, proved treacherous in unpredictable ways. Later, practitioners confronted allergic reactions, rare genetic disorders like malignant hyperthermia, and the need for constant monitoring.
Have you ever wondered about the ethical questions that anesthesia stirred? Some early religious leaders opposed it, arguing that suffering was part of the human experience. Only after public successes — and royal endorsements — did views shift toward compassion and relief. The legitimacy of anesthesia wasn’t guaranteed. It was hard won, trial by trial, patient by patient.
Fast forward to the present day, and the very concept of pain in surgery seems distant. Techniques have expanded further: spinal anesthesia, regional nerve blocks, patient-controlled devices, and even computer-guided systems that adjust dosages in real time. I often think about how this evolution mirrors changing human values. Where once stoicism ruled, today the goal is dignity, comfort, and measurable safety.
Do you ever stop to think how this journey will continue? Anesthesiologists now experiment with non-opioid drugs, individualized genetic testing, and virtual reality tools to prepare patients psychologically. As robotic surgery and minimally invasive techniques advance, the demand for adaptable, gentle anesthesia only grows.
We began with a simple quest to ease pain. Now, the field is marked by a relentless drive for precision and compassion. Think about that the next time you sign a surgical consent: you are the beneficiary of centuries’ worth of urgency, debate, and ingenuity.
“Nothing in life is to be feared, it is only to be understood.” Marie Curie’s famous statement resonates powerfully here. Anesthesia, once feared for its unpredictability, has become a beacon of scientific understanding and empathy.
So, the journey from raw pain to peaceful sleep transformed the very intention of surgery. Patients are no longer victims but collaborators, surgeons are freed to focus on skill rather than speed and brute force, and the unpredictable suffering of the operating room has faded into history. The arc of anesthetic progress is not just a medical story. It captures the enduring human hope that science and compassion can become one.